Mental Models and Creating Culture Change
Designing the way we see and think

Welcome to the Design Loft!
You might have heard about mental models. Today, we’re going to discuss them and what they mean for creating change, by design.
Key Takeaways:
Mental models are the unconscious frameworks that shape how you diagnose problems and design solutions in your health practice. While your professional training provides essential defaults—protocols for physicians, assessment tools for social workers, policies for administrators—these same mental models can limit your effectiveness by creating confirmation bias, tunnel vision around familiar solutions, and blind spots to equity or systemic issues. To unlock better outcomes, make these invisible assumptions visible through tools like assumption mapping and journey mapping, bring lived experience from patients and frontline staff into decision-making, challenge dominant narratives with fresh evidence, and use small prototypes as learning experiments rather than proof-of-concept exercises. The goal isn’t to abandon your professional expertise but to consciously examine which mental models serve your work and which need refreshing—because shifting how you see problems often reveals solutions that were always possible but previously invisible.
Mental Models: Introduction
Mental models are the invisible frameworks people use to understand the world and decide how to act. They are the defaults for beliefs or lenses through which we see things. In design for health and social impact, mental models shape how leaders interpret problems, value evidence, and imagine what is possible. Because these models guide behaviour and decisions, practical design work often begins by making them visible so we can be more conscious of our thoughts, actions, and creative potential.
Simple Definition:
A mental model is a set of assumptions, beliefs, and expectations that people use—consciously or unconsciously—to make sense of complex situations and choose a course of action.
Why They Matter in Strategic Design & Health:
They influence how teams diagnose problems and whether they see systems or symptoms or whether they see policies or people.
They affect openness to change—especially in complex, high-stakes environments like health and social services.
Shifting mental models can unlock new pathways for innovation, collaboration, and impact.
They can create efficiencies and also limit effectiveness (depending on how they’re used)
They shape who and what we design for (and who we exclude)
Mental models act like lenses on the world around us. They help us navigate complexity, but they can also narrow our field of vision. In health and social impact work, this has real consequences: leaders may focus on familiar and outdated solutions, overlook root causes, or assume constraints that no longer exist.
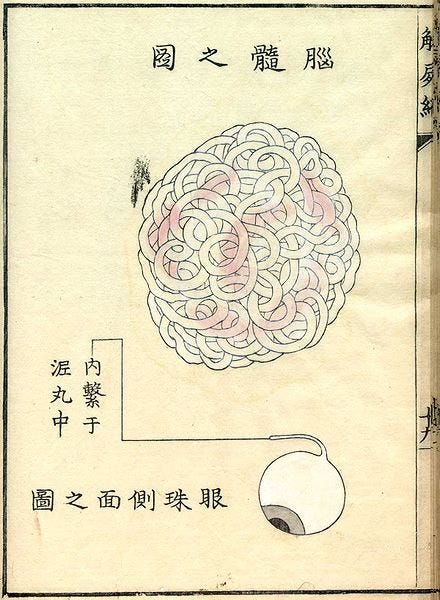
Mental models reflect the discipline of our practice.
Physicians are trained on protocols.
Social Workers learn to see signs in behaviour and employ assessment tools.
Administrators rely on policies.
Funders look to the numbers.
These can provide a touchstone for guidance in certain situations. In design, our role is to question these to see the value they create and the unrealized value they leave behind. We designers aim to create solutions, and that might mean changing people’s mental models.

Common Ways Mental Models Limit Action
How do you spot where mental models come into play?
Confirmation loops: We notice evidence that fits our existing beliefs and ignore what challenges them.
Default solutions: We rely on what has worked before, even when the context has changed.
Invisible assumptions: We inherit norms (“that’s just how it’s done in healthcare”) that quietly block innovation.
Tunnel vision: Professional training and organizational culture can create blind spots around equity, community experience, or systemic drivers.
Risk misperception: Long-standing beliefs about what is “too risky” or “not possible” prevent experimentation—even when evidence says otherwise.
These limitations are not flaws in individuals—they are predictable outcomes of working in complex, fast-changing systems.
⸻
How to Overcome Limiting Mental Models in Health & Social Impact
1. Make the Invisible Visible
Use tools like assumption mapping, systems mapping, journey mapping, or pre-mortems to surface the beliefs that guide decisions.
If we can’t name it, we can’t change it.
2. Bring Lived Experience into the Room
Engage patients, communities, and frontline staff. Their perspectives reveal where long-held institutional or disciplinary assumptions fail. They are at the front of what’s going on; create the means to listen to and engage these perspectives.
Diverse viewpoints expand the mental model of the system.
3. Use Evidence as a Disruptor
Present data that challenges dominant narratives—especially around equity, outcomes, or how change happens. We often fail to ‘refresh’ our evidence base. Conduct periodic updates to see what the latest evidence says, and look for where there are gaps -- and where there are fillers.
Well-placed evidence can reframe what leaders believe is possible.
4. Prototype to Learn, Not to Prove
Small, low-risk experiments help teams test assumptions and update their mental models quickly. Prototypes help us develop new things, but their primary benefit is to facilitate learning through making and building praxis (reflective learning through action).
Doing creates new understanding that thinking alone cannot.
5. Create Reflective Leadership Practices
Build pauses into decision-making using tools like after-action reviews, reflection prompts, and strategic design sprints to help teams examine their thinking.
Reflection lets leaders adjust course before systems drift too far.
6. Introduce Alternative Models and Narratives
Strategic design provides new ways of seeing problems (e.g., systems thinking, human-centred design, complexity science).
When a better mental model becomes available, people adopt it. If you design for adoption and implementation at the outset, you increase the receptor capacity and likelihood of creating change that sticks.
Alternatives allow for different stories to be told.
⸻
Now, could you get out there and design for the models you have and the ones you need to cultivate? Do it! Let me know how it goes.
What mental models do you use in your practice? Which ones are the most helpful? Which ones might need a refresh?
For Premium and Paid Subscribers, read on to see case studies of how and where this approach has been used. If you’re interested in becoming a paid subscriber, click the link below and elevate your design practice even more.
If what you need is help putting this into practice, reach out and let’s talk (click below)
Thanks for reading.
References
Wikipedia – Mental Model: https://en.wikipedia.org/wiki/Mental_model
Johnson-Laird, P. (1983). Mental Models. Harvard University Press.
Parrish, S. (2023) Mental Models: The Best Way to Make Intelligent Decisions (~100 Models Explained) https://bit.ly/4o6pTvY
Keep reading with a 7-day free trial
Subscribe to The Design Loft to keep reading this post and get 7 days of free access to the full post archives.